GeneSafe
GeneSafe – a non-invasive prenatal screening test
This blood test is designed to measure the combined maternal and fetal DNA present in maternal blood and is considered a genetic test. Your written consent is required to perform a genetic test.
To analyze the DNA from your blood, your health care provider will take a blood sample from you (two tubes between 7 and 10mL, in a standard blood draw). The physical risk to you of obtaining the blood sample is usually minimal.
Circulating cell-free fetal DNA is first purified from the plasma component of anti-coagulated maternal whole blood.
Through a state-of-the-art technological process, named Next Generation Sequencing (NGS) technique, 29 genes are completely sequenced (exons and adjacent intronic regions, ± 5 nucleotides) at high read depth (>500X). The resulting genetic sequences are analysed via an advanced bioinformatics analysis, to check for the presence of potential mutations in the genes under investigation.
GeneSafe de novo screens for 44 severe genetic disorders due to de novo mutations (a gene mutation that is not inherited) in 25 genes that cause skeletal dysplasia, congenital heart defects, multiple congenital malformation syndromes, neurodevelopmental disorders, such as autism,
epilepsy, intellectual disability and sporadic cases of various rare dominant Mendelian disorders, such as Kabuki syndrome, Schinzel-Giedion syndrome and Bohring-Opitz syndrome. The rate of de novo variants has been shown to increase as paternal age advances. The 44 different disorders screened by this innovative test often occur in the absence of a family history of the condition.
The conditions screened meet at least one of the following criteria:
- Cause cognitive disability
- Require surgical or medical intervention
- Affect quality of life
GeneSafe Inherited screens for 5 common inherited recessive genetic disorders, such as Cystic Fibrosis, Deafness autosomal recessive type 1A, Deafness autosomal recessive type 1B, Thalassemia-Beta, Sickle cell anemia. While the results of the prenatal test are highly accurate,discordant results may occur. Cell-free DNA (cfDNA) testing does notreplace the accuracy and precision of prenatal diagnosis with CVS or amniocentesis.
Service providers
| Service | Price |
|---|---|
GeneSafe De Novo | 900€ |
GeneSafe De Novo + Gene Inherited | 1000€ |
What is Intralipid?
Evidence from both animal and human studies suggest that intralipid administered intravenously may enhance implantation. Intralipid is a 20% intravenous fat emulsion used routinely as a source of fat and calories for patients requiring parental nutrition. It is a synthetic product composed of 10% soybean oil, 1.2% egg yolk phospholipids, 2.25% gylcerine and water. Intralipid infusions stimulated the immune system to remove “danger signals” that can lead to pregnancy loss. The appeal of Intralipid lies in the fact that it is relatively inexpensive and is not a blood product.
This product is given by injection into a vein as directed by your doctor.
In 2011, UK researchers gave intralipid infusions to 50 women. All had endured numerous unsuccessful IVF cycles. Half of them got pregnant after taking the intralipids. The miscarriage rate was higher for another group who weren’t given intralipids. Small study, but an interesting one.
Some doctors think natural killer (NK) cells in the body attack embryos and that intralipids stop that happening. But larger randomized trials into IVF and intralipids are needed to really prove this.
The truth is, intralipids might help. Might. Not will. If you’ve had miscarriages, repeated implantation failure and have elevated NK levels, intralipid infusion therapy will be on your clinic’s price list.
A typical course of IVF intralipid treatment is two infusions: the first one 7 to 10 days before your scheduled egg retrieval; the second on your embryo transfer day. Some clinics propose a third infusion after a positive pregnancy test and monthly ones till the 13-week mark.
Intralipid infusions as treatment for recurrent unexplained abortion?
It can be hypothesized from the human clinical trial data that Intralipid even in small doses could be an effective antiabortion treatment. The number of patients in the published study is too small for the required degree of precision. Intralipid was highly effective in preventing abortion in mice, and protection was prolonged. This may be explained by previous data in the literature showing that Intralipid affects the reticuloendothelial system of the recipient. CONCLUSIONS: The evidence suggests that Intralipid might be an effective treatment for human recurrent miscarriages, and injection into women who may become pregnant has been found ethically acceptable at one university center. Comparison of Intralipid to partner leukocyte immunotherapy or IVIG would be worthwhile. For adequate statistical power, this would require a large, multicenter, prognostically stratified randomized controlled trial.
Intralipid is effective in enhancing live birth rates among women with elevated NK cell cytotoxicity and a history of recurrent implantation failure and recurrent pregnancy loss.
Intralipid is effective in suppressing in vivo abnormal NK-cell functional activity. The results suggest that Intralipid can be used successfully as a therapeutic option to modulate abnormal NK activity in women with reproductive failure.
Possible side effects of intralipid infusions.
Headache, dizziness, flushing, drowsiness, nausea, vomiting or sweating may occur. If any of these effects persist or worsen, tell your doctor promptly.
Remember that your doctor has prescribed this medication because he or she has judged that the benefit to you is greater than the risk of side effects. Many people using this medication do not have serious side effects.
Tell your doctor right away if any of these unlikely but serious side effects occur: signs of infection (e.g., fever, persistent sore throat), pain/swelling/redness at injection site, pain/swelling/redness of arms/legs, bluish skin, sudden weight gain, shortness of breath, back/chest pain.
Tell your doctor right away if any of these rare but very serious side effects occur: mental/mood changes, bone pain, muscle weakness, yellowing skin/eyes, dark urine, easy bruising/bleeding, severe stomach/abdominal pain, trouble breathing.
A very serious allergic reaction to this drug is rare. However, seek immediate medical attention if you notice any symptoms of a serious allergic reaction, including: rash, itching/swelling (especially of the face/tongue/throat), severe dizziness, trouble breathing.
This is not a complete list of possible side effects. If you notice other effects not listed above, contact your doctor.
Precautions before using intralipid infusions.
Intralipid infusions should not be used if you have certain medical conditions. Before using this product, consult your doctor or pharmacist if you have: high fat (lipid) levels in the blood.
Before using this medication, tell your doctor or pharmacist your medical history, especially of: severe liver disease, kidney disease, lung disease, anemia, blood clotting disorder.
During pregnancy, this medication should be used only when it is clearly needed. Discuss the risks and benefits with your doctor.
It is not known whether this drug passes into breast milk. Consult your doctor before breast-feeding.
Operative surgery plays an important role in infertility treatment and in vitro fertilization. It is often believed that unsuccessful ET is connected to bad quality of embryo. In that case it is forgotten that there are three main factors that are relevant for becoming pregnant – embryo, uterus and body. In this article we focus on factors connected to uterus.
Which factors are considered to be important so that uterus would accept embryo(s)? These factors are correct structures and function of uterus and endometrial fluid.
Mostly the changes of uterus are connected to woman`s age. Women older than 35 years are more likely to have such changes in their uterus as myomas, adenomyosis, polyposis of endometrium or endometrial hyperplasia. Often these changes are caused by long term hormonal treatments during numerous unsuccessful IVF attempts and every change could be a factor impacting embryo implantation. Also chronic flammatory processes in uterus, fallopian tubes and in small pelvis may be the reasons why women cannot get pregnant.
Before operative treatment is put into practice there is a need to make certain that microflora of vagina is in normal range.
Operative surgery – hysteroscopy and laparoscopy
There is used laparoscopic and hysterescopic surgery for operative treatment.
During hysterescopy it will be controlled if the uterine cavity is big enough, if there are abnormalties of uterus (for example septum of the uterus, bicornuate uterus), submucosal myomas of uterus, polyps, endometrial hyperplasia, adhesions and the changes are tried to be corrected.
During laparoscopy there will be controlled the possible changes of small pelvis. Mostly among infertile patients there are found lesions of endometriosis and removing those may reduce the impact of endometriosis on uterus and function of fallopian tubes and ovaries.
In case there is chronic inflammation in fallopian tubes and they have been operated before and the restoration of their function was not successful, removing the fallopian tubes that have such changes may increase the chances to become pregnant after embryo transplantation.
One of the reasons why embryo transplantations have not been successful may also be big, intramural and subserosally located myoma knots with a diameter 5 cm and more, they can be removed laparoscopically. Correction of adhesions in small pelvis may repair the function of organs.
Service Providers
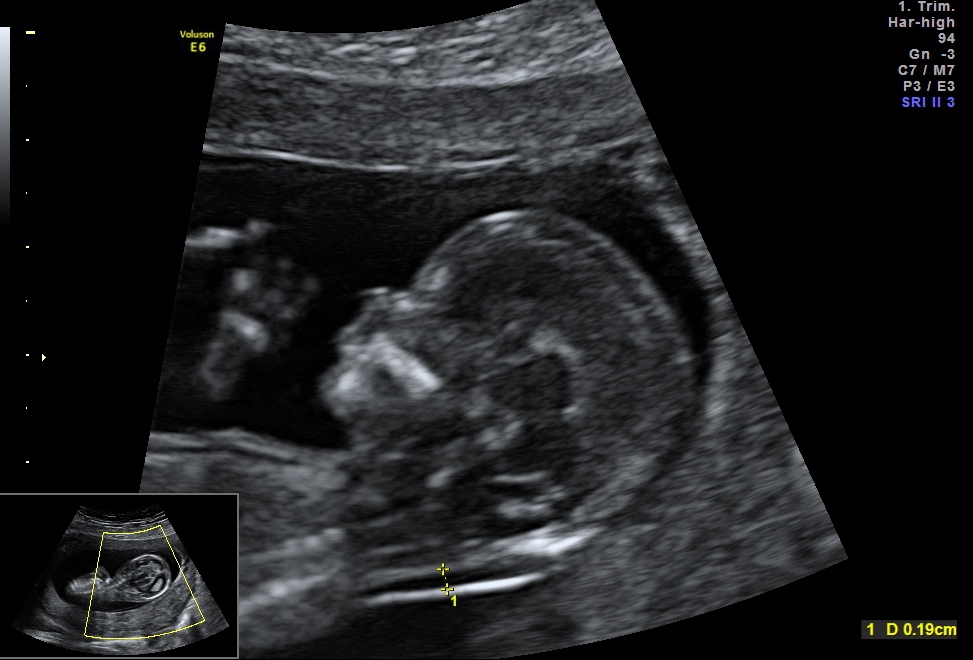
4D Ultrasound at Different Stages of Pregnancy – What to Expect?
- 4D ultrasound at 11–14 weeks of pregnancy – includes nuchal translucency measurement
- 4D ultrasound at 15–18 weeks of pregnancy – possible to determine the baby’s sex
- 4D ultrasound at 23–27 weeks of pregnancy – the best time to visualize the baby’s facial features
What’s Included in the 4D Ultrasound:
- Measurement of the baby
- Visualization of fetal movements
- Visualization of the fetal heartbeat and heart rate measurement
- Visualization of limbs
- Determination of placenta position
- Measurement of amniotic fluid
- Visualization of the spine
- Fetal anatomy assessment (if selected by the patient)
- Ultrasound summary and video clips
- Images on a USB stick, if the baby’s position allows for good imaging
Note: Image quality depends on the baby’s position during the scan.
Recommendations:
- Please bring your maternity card to the appointment.
- From week 15 onwards, remove any belly button piercings before the scan.
- Starting at week 15, we recommend increasing fluid intake in the week leading up to the scan.
Greater fluid intake before a 4D ultrasound increases the chances of capturing clear facial images. If there’s more amniotic fluid, it’s even possible to get good facial pictures up to week 31.
That’s why we suggest drinking an extra liter of water per day (or similar fluids) for one to two weeks before your 4D ultrasound.
Note: Increased fluid intake is relevant starting from week 15 ultrasounds and beyond.
Service providers
Service providers are dr Deniss Sõritsa ja dr Andrei Sõritsa. For these scans, we use the high-quality Voluson E10 ultrasound system, ensuring detailed and clear imaging.
Upon request, images and video clips can be saved to a USB stick by the doctor.
| Booking | |
|---|---|
Broneeri iseteeninduses |
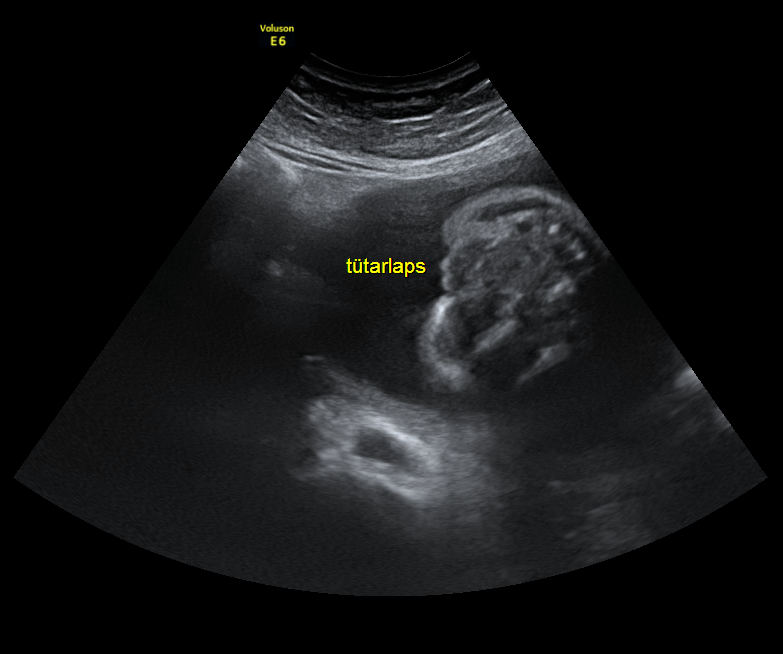
Ultrasound Examination at 11–13 Weeks of Pregnancy
Ultrasound Examination at 11–13 Weeks of Pregnancy Includes:
- Measurement of nuchal translucency
- Visualization of fetal movements
- Measurement of the fetus
- Visualization of the fetal heartbeat
- Visualization of limbs
- Determination of the placenta’s position
- Measurement of amniotic fluid volume
- Visualization of the spine
- Basic fetal anatomy assessment
For more information, please contact the Elite Clinic reception.
Service providers:
The 11–13 week ultrasound examination is performed by Dr Deniss Sõritsa, Dr Mare Riive, Dr Svetlana Räim, and Dr Andrei Sõritsa, all of whom hold a valid FMF (Fetal Medicine Foundation) license.
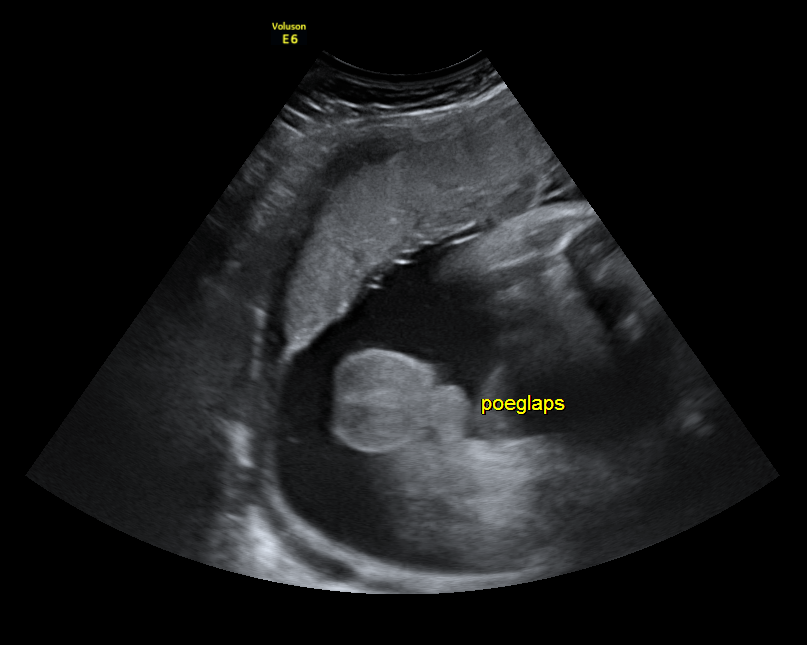
Ultrasound Examination at 19–20 Weeks of Pregnancy
The fetal anatomy scan is a crucial and comprehensive assessment of the baby’s body and organ development. It helps identify possible developmental abnormalities and structural defects, and if necessary, allows for further testing and planning of care.
The Ultrasound Includes:
- Fetal anatomical assessment
- Visualization of fetal movements
- Fetal measurements
- Visualization of fetal heartbeat and heart rate measurement
- Visualization of limbs
- Placenta location determination
- Amniotic fluid level assessment
- Spinal cord visualization
- Determining the baby’s position
- Visualization of the baby’s sex
Please note: Not all existing fetal abnormalities can be detected during the 19–21 week scan. Even if no immediate medical indication arises after 21 weeks, we recommend all pregnant women undergo additional follow-up scans between: * Weeks 24–27 , to assess overall fetal development, internal organs, and organ function (this is also the ideal time for a 3D–4D ultrasound – [INSERT ACTIVE LINK] – which can help detect subtle anomalies such as cleft palate, limb malformations, or heart defects)
Even if both first and second trimester scans show low risk for fetal anomalies, it is important to understand that they do not guarantee the birth of a completely healthy baby. Some conditions can only be detected in the third trimester, and others may not be diagnosed until after birth.
Service providers:
The 19–20 week ultrasound examination is performed by Dr Deniss Sõritsa, Dr Mare Riive, Dr Svetlana Räim, and Dr Andrei Sõritsa
Ultrasound Examination from 36 Weeks of Pregnancy Onwards
A third-trimester ultrasound plays a key role in assessing the baby’s growth, position, and well-being — helping both the expectant mother and healthcare provider prepare for birth.
The Ultrasound Includes:
- Assessment of the baby’s position
- Estimated fetal weight (birth weight prediction)
- Measurement of amniotic fluid volume (AFI – Amniotic Fluid Index)
- Umbilical cord Doppler ultrasound (assesses oxygen and nutrient supply to the baby)
- Visualization of fetal heartbeat and heart rate measurement
- Observation of fetal movements
- Visualization of limbs and spine
- Placenta location assessment

Elite Clinic recommends a pre-delivery ultrasound, as it provides crucial information on possible fetal abnormalities, low birth weight, changes in umbilical blood flow and abnormal levels of amniotic fluid.
This examination helps determine whether intervention (e.g., labor induction) may be needed.
It also offers early insight into whether the baby might require surgery or special care after birth, allowing for appropriate planning before labor begins.
Additionally, the scan helps evaluate if the delivery should take place in a Level III (highest level) medical facility. If a fetal abnormality is detected, early decisions can be made regarding the mode of delivery and postnatal treatment, ensuring the best possible care pathway.
Service Providers
dr Mare Riive, dr Deniss Sõritsa ja dr Andrei Sõritsa.
| Booking | |
|---|---|
Broneeri iseteeninduses |
The first step is to determine the length of the functional part of the fallopian tube and the location of the blockage. This can be done either with an ultrasound (HyCoSy ultrasound) or with an X-ray examination (hysterosalpingography).
The surgery is performed under general anesthesia, either laparoscopically or via a conventional open approach.
After the procedure, patients usually experience mild discomfort, which can be managed with pain medication.
Following laparoscopic surgery, the patient can go home the same day and typically resumes normal activities within about a week.
After conventional surgery, hospital stay is usually required for 4–6 days, and recovery takes 4–6 weeks.
Couples are advised to try to conceive within 6–12 months after sterilization reversal, as the surgery can lead to the formation of scar tissue that may block the fallopian tube.
Service Provider
Price
| Nimetus | Price |
|---|---|
Price | Starting from 3200€ |
Teenuseosutajad
Before Termination of Pregnancy
At the first visit, the doctor confirms the pregnancy and its duration, orders necessary tests and, if needed, treatment, and counsels the person seeking a termination.
To avoid complications related to abortion, we recommend the patient agrees to the prescribed tests, examinations, and treatments.
It is important to inform the doctor confirming the pregnancy about:
- your current health status;
- all past and present illnesses;
- any medications being taken;
- any known drug allergies.
Surgical Termination of Pregnancy
Surgical abortion is the termination of pregnancy using a surgical method.
The procedure is preceded by a gynecological examination. Under short general anesthesia, the cervix is dilated and the pregnancy is terminated using vacuum aspiration. Sometimes, cervical preparation is required beforehand—medication is administered vaginally or sublingually.
On the morning of the procedure:
- Do not eat or drink;
- Do not chew gum or smoke;
- If you have a chronic illness (e.g., hypertension, asthma) and are on prescribed medications, you must still take your usual morning doses. A small sip of water for swallowing pills is allowed and safe. Some diabetes medications may be an exception and should not be taken without food;
- Empty your bladder before the procedure.
After the Procedure
After the procedure, the patient remains for a couple of hours in the operating unit on the second floor for observation until the effects of anesthesia subside and pain is under control. Before discharge, the nurse will remove the IV cannula. A sick leave certificate may be issued if needed.
Possible Complications of Surgical Abortion and When to Seek Emergency Help
Abortion is generally a safe procedure. However, the following complications are possible:
- Ongoing pregnancy (occurs in <1:100 cases) — the procedure must be repeated;
- Incomplete abortion (2:100)‒ Incomplete abortion (2:100) — the procedure must be repeated;
- Bleeding >500 ml (risk of transfusion-requiring bleeding is <1:1000);
- Uterine perforation (1–4:1000);
- Cervical injury (<0.2:100);
- Pelvic inflammatory disease, usually caused by pre-existing sexually transmitted infection (can increase risk of future tubal infertility or ectopic pregnancy). To reduce this risk, STI testing is done before the abortion, and treatment or prophylactic antibiotics are recommended if needed;
- Anesthesia-related complications, primarily drug hypersensitivity (0.5:10,000).
In rare cases (e.g., cervical injury, uterine perforation, significant bleeding), surgical intervention (laparoscopy or open surgery) may be required.
Seek emergency gynecological care or visit the 24/7 emergency department of a tertiary care hospital if you experience:
- Severe or increasing pain;
- Bleeding heavier than a normal period or lasting more than two weeks;
- Fainting;
- Vomiting;
- High fever (>24 hours), chills;
- Foul-smelling or purulent vaginal discharge.
If you suspect the pregnancy may be continuing (e.g., breast tenderness and enlargement, nausea/vomiting, fatigue, changes in appetite, frequent urination), contact a gynecologist immediately.
After Surgical Abortioni
The need for a follow-up visit is determined by the doctor, taking the patient’s wishes into account.
If the abortion proceeds without complications, a follow-up visit may not be necessary.
For two weeks after the abortion, we recommend avoiding unprotected sex, tampons, baths, and swimming.
Your next menstrual period should start within 4–6 weeks. If it does not, consult a gynecologist.
Avoiding Unintended Pregnancy
Fertility returns immediately after a pregnancy termination, so to prevent a new pregnancy, it is essential to begin using an effective contraceptive method either before or immediately after the abortion.
Hormonal contraceptive methods (such as pills, patch, vaginal ring, mini-pills, implant, or injectable progestogens) are typically started on the same day as the abortion.
An intrauterine device (IUD) may also be inserted by a doctor during the abortion procedure.
You can discuss suitable contraceptive options with your doctor prior to the abortion.
Teenuseosutaja

Anne Lepasepp
Physiotherapist
Teenuseosutaja
Teenuseosutaja
Teenuseosutaja
Teenuseosutaja
HPV (Human Papilloma Virus)on inimeselt-inimesele leviv viirus, mis võib põhjustada healoomulisi muutusi nahal (nt soolatüükaid) ja limaskestadel (nt teravad kondüloomid). Mõned papilloomiviiruse tüübid võivad põhjustada ka pahaloomuliste kasvajate teket genitaalpiirkonnas ning suuõõnes. Neli inimest viiest nakatub elu jooksul HPV-sse.
HPV vaktsiin on põhjalikult uuritud ja see on ohutu, kõrvaltoimeid esineb väga harva ning need on kerged. Tegutse kohe, sest nii ennetad rasket haigust ja aitad muuta Eesti tervemaks.
Emakakaelavähk on rahvusvahelise vähiuuringute agentuuri andmetel maailmas neljas kõige levinum vähk naiste seas. 2020. aastal avastati maailmas hinnanguliselt üle 600 000 uue emakakaelavähi juhu ning selle tõttu suri üle 300 000 naise.
Eestis on viimase paarikümne aasta jooksul püsinud nii emakaelavähki haigestumus kui ka suremus suhteliselt muutumatuna. 2020. aastal tuvastati Eestis 116 uut emakakaelavähi juhtu. Soomes püsib haigestumus ligi 4 korda madalam. Eestis suri 2020. aastal emakakaelavähi tõttu 64 naist. Enim juhte diagnoositakse Eestis peale 55. eluaastat.
Kui oled huvitatud HPV vastu vaktsineerimisest, palume esmalt pöörduda naistearsti vastuvõtule.
Teenuseosutaja
Service Provider

Lemme Haldre
Clinical psychologist
Haava pind paraneb kurgus u 12-14 päeva, sel perioodil on verejooksu oht. Lõikusest taastumise perioodil on vajalik süüa pehmet jahedat toitu ja juua sageli jahedat vett. Oluline on ka suu puhtuse eest hoolitsemine ja regulaarne hambapesu.
Kurguvalu on sel ajal tavapärane, valu saab leevendada valuvaigistitega, soovitame vees lahustuvaid tablette.